Bone Density and Osteoporosis in Menopause: Your Guide to Prevention and Treatment

- Remove the existing class from the content27_link item to allow Webflow's native current state to be applied automatically.
- To implement interactions that allow sections in the table of contents to expand and collapse, select the content27_h-trigger element, add a trigger, and choose Mouse click (tap).
- For the first click, select the custom animation Content 28 table of contents [Expand], and for the second click, choose the custom animation Content 28 table of contents [Collapse].
- In the Trigger Settings, ensure that all checkboxes are deselected except for Desktop and above to prevent interaction issues on tablet and smaller devices.
Introduction: The Invisible Threat to Menopausal Women
Menopause is a natural and inevitable phase in a woman's life. While symptoms such as hot flushes and mood swings often get attention, a quieter but potentially much more profound change is taking place in the background: the decline in bone density. This process, known as osteoporosis, can lead to osteoporosis, a condition that weakens the skeletal system and dramatically increases the risk of bone fractures. It is estimated that over 1 million people in the Netherlands osteoporosis, and this number is expected to increase. The impact is significant; recent research shows that the number of new fragility breaches worldwide has increased by 33.4% over the past 30 years.
What is bone loss and why is it so relevant during menopause?
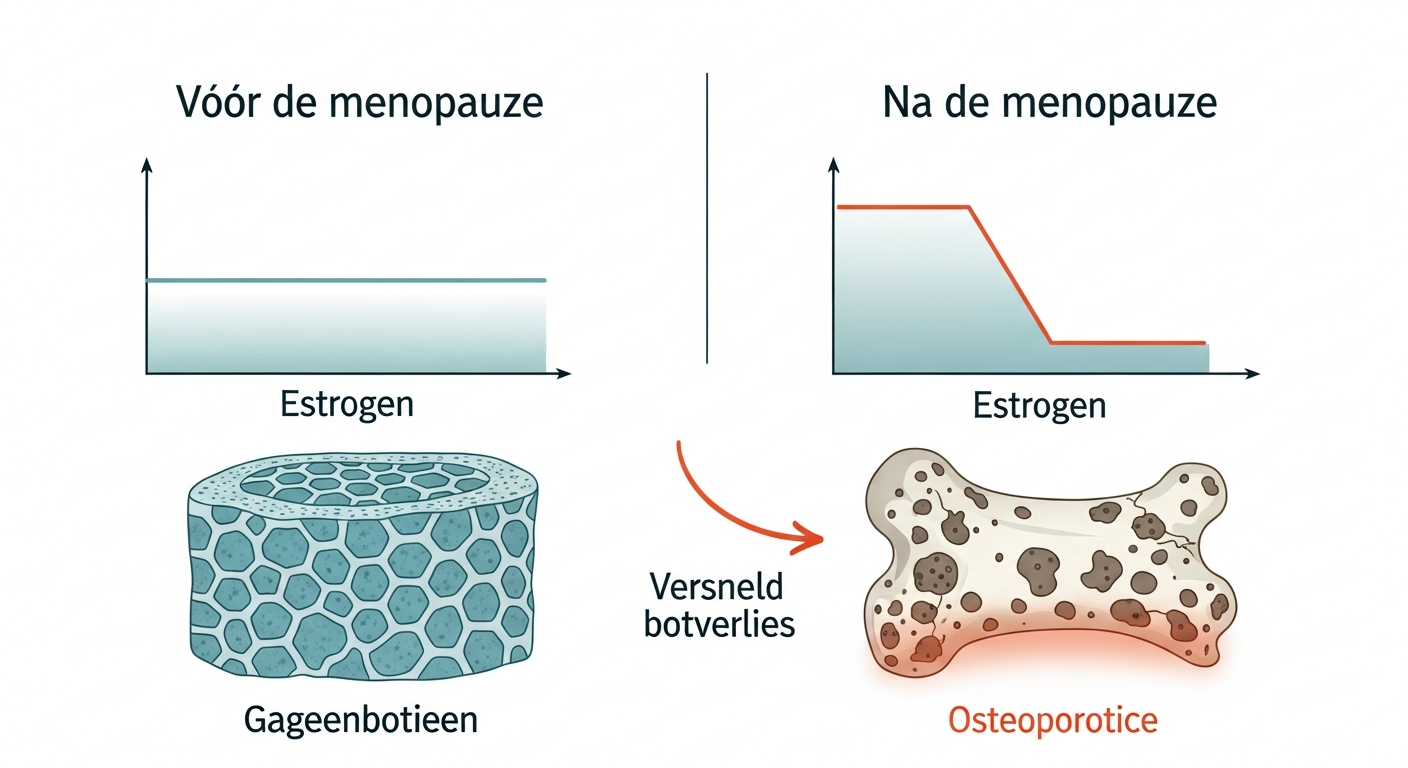
The drop in estrogen during menopause accelerates bone loss, changing bone structure from dense and strong (left) to porous and fragile (right).
Bone loss is a natural part of the aging process. However, during and after menopause, this process undergoes significant acceleration. The cause lies in the sharp decline in the hormone estrogen, which plays a crucial protective role in maintaining bone mass. This accelerated loss significantly increases the risk of osteoporosis. Because osteoporosis often causes no symptoms until a fracture occurs, it is also known as the “silent disease”. For menopausal women, awareness and proactive action are therefore essential to face the invisible threat of bone loss.
What do you learn in this guide? A practical approach to prevention and treatment
This guide provides a complete overview of the relationship between menopause, bone density and osteoporosis. We'll dive into the biology of bone tissue, the impact of hormonal changes, and the risk factors you need to know. More importantly, we offer concrete, evidence-based strategies for prevention through diet, exercise, and lifestyle changes. In addition, we discuss diagnostic methods, such as the DEXA scan, and available treatment options, from medication to supportive therapies. The goal is to provide you with the knowledge and confidence to take control of your bone health, now and in the future.
Understanding Bone Health: The Foundations of Strong Bones
To understand the impact of menopause, it's crucial to first know how bones function. The skeleton is not a static structure, but a dynamic, living organ that is constantly being renewed. This insight forms the basis for effective prevention and treatment of bone loss.
The Architecture of Bones: More than Just Hardness
Bone tissue consists of a matrix of collagen (which provides flexibility) and minerals, primarily calcium phosphate (which provides hardness and strength). This combination makes bones both strong and resilient, able to withstand the forces of daily life. Bone Mineral Density (BMD) is a measure of the amount of minerals in a given volume of bone. Higher bone density generally means stronger bones. During childhood and early adulthood, more bone mass is built up than broken down, resulting in a peak bone mass around the age of 30. This peak is a crucial determinant for the risk of osteoporosis later in life.
Bone Conversion: A Lifelong Process of Degradation and Building
The process of bone renewal is called “bone conversion” or “remodeling.” Old, damaged pieces of bone are continuously removed by specialized cells called osteoclasts (bone breakdown), then new, strong pieces of bone are formed by cells called osteoblasts (bone structure). In a healthy, young body, these two processes are perfectly balanced. This cycle ensures that the skeleton can adapt to stress and repair minor damage. After the menopause, however, this balance is disturbed, with bone degradation prevailing over the build-up.
What is Osteopenia and Osteoporosis? The Different Stages of Bone Loss
When bone density decreases but is not so severe that osteoporosis occurs, this is called osteopenia. It is a warning phase that indicates that the bones are getting weaker and the risk of fractures is increasing. Osteoporosis, literally “porous bone,” is a more advanced stage of bone decalcification. Here, the bone mass and the structural quality of the bone tissue are reduced to such an extent that even a minor fall or a slight impact can cause a fracture. Typical osteoporotic fractures include those of the wrist, vertebrae, and hip.
Menopause as a Tipping Point: Hormonal Changes and Bone Loss
Menopause marks a significant tipping point for a woman's health, particularly her skeletal system. The hormonal shifts that characterize this period have a direct and profound impact on the rate of bone loss.
Estrogen: The Key to Bone Health
Estrogen plays a central role in regulating bone turnover. This hormone acts as a natural brake on the activity of osteoclasts, the cells responsible for bone degradation. By controlling osteoclasts, estrogen ensures that bone structure can keep up with the breakdown, so that bone mass is maintained. It also helps absorb and utilize calcium, an essential building block for strong bone tissue.
The Impact of Hormonal Changes During Menopause
During perimenopause and menopause, the production of estrogen by the ovaries drops drastically. This drop in estrogen levels releases the brakes on osteoclasts. The result is a period of accelerated bone degradation. The osteoblasts (bone-building cells) cannot keep up with this pace, leading to a net loss of bone mass. This process is most intense in the first five to seven years after the last menstrual period. Research shows that women can lose 40-50% of their bone mass in their lifetime, which explains why 1 in 4 women over the age of 50 develops osteoporosis.
The Long Term Consequences: An Increased Risk of Fractures
The direct result of this accelerated bone loss is a weakened skeleton and a significantly increased risk of fractures. Globally, it is estimated that 1 in 3 women and 1 in 5 men over 50 suffering from osteoporotic fractures. A vertebral fracture (sagging fracture) can lead to chronic pain, loss of height and a hunched posture (kyphosis). A hip fracture is often the most disabling and can lead to loss of independence, the need for long-term care and even an increased risk of mortality. Prevention and early diagnosis are therefore crucial to prevent these serious consequences.
Osteoporosis Risk Factors: What You Need to Know
While menopause is a universal risk factor for women, there are numerous other factors that can influence the chances of developing osteoporosis. Understanding your personal risk profile is the first step towards effective prevention.
Immutable Risk Factors
Some risk factors are genetic or biologically determined and cannot be changed. However, it's important to know them:
- Gender: Women naturally have a lower peak bone mass than men and experience accelerated bone loss during menopause. Osteoporosis affects 22 million European women over the age of 50.
- Age: The risk of osteoporosis increases with age, as bone density gradually decreases after the age of 35.
- Ethnicity: White and Asian women have a higher risk than dark-skinned women.
- Family history: If one of your parents has had a hip fracture, or if osteoporosis runs in the family, your deductible is increased.
- Body type: A petite build and a low body weight (BMI < 19) are associated with lower bone mass.
- Early menopause: Menopause before age 45 (naturally or through surgery) means a longer period of low estrogen levels.
Lifestyle Factors That Wreck Bone Loss
Many risk factors are related to lifestyle and can thus be influenced:
- Tuxedo: Smoking has a direct toxic effect on bone building cells. It can also lead to an earlier menopause and reduces calcium absorption.
- Excessive alcohol consumption: More than two units of alcohol a day can interfere with bone formation and increases the risk of falls.
- Sedentary lifestyle: Lack of weight-bearing exercise leads to a decrease in bone strength, because bones lack the mechanical stimulus necessary for the production of new bone tissue.
- Inadequate intake of calcium and vitamin D: These nutrients are essential for building and maintaining bones. A chronic deficiency inevitably leads to bone loss.
Medical Conditions and Medications
Certain diseases and medications can negatively affect bone metabolism and increase the risk of secondary osteoporosis:
- Medical conditions: Rheumatoid arthritis, Crohn's disease, celiac disease, hyperthyroidism (overactive thyroid), and kidney disease can affect bone health.
- Medication: Long-term use of corticosteroids (such as prednisone) is a known cause of medication-induced osteoporosis. Certain antiepileptic drugs and medications used to treat breast and prostate cancer can also reduce bone density.
Early Detection: The Diagnosis of Osteoarthritis
Because osteoporosis is a silent condition, early and accurate diagnosis is vital. Waiting for a fracture is not an effective strategy. Proactive screening among women at risk can make the difference between maintaining mobility and experiencing a disabling breakup.
When to sound the alarm Symptoms and Indicators
In the early stages of bone loss, there are usually no symptoms. However, as the bones become weaker, indicators may appear that warrant further investigation:
- A bone fracture after a minor fall or impact (a fragility fracture).
- Loss of body height (more than 3-4 cm).
- Sudden, severe back pain with no apparent cause, which may indicate a collapsed vertebra.
- Developing a more curved posture (a “crooked back”).
If you experience one or more of these indicators, or if you have multiple risk factors, it is recommended that you discuss this with your doctor.
The Gold Standard: The DEXA Scan
The most reliable method for measuring bone density is the Dual-Energy X-ray Absorptiometry, better known as the DEXA scan. This is a quick, painless and safe procedure that uses a very low dose of X-rays to measure the amount of bone mineral in the hip and lumbar spine. These are the locations where osteoporotic fractures are common and have the biggest impact.
The results of a DEXA scan are expressed as a T score. This score compares your bone density to the average peak bone mass of a healthy young adult of the same sex.
- T score of -1.0 or higher: Normal bone density.
- T score between -1.0 and -2.5: Osteopenia (decreased bone density).
- T score of -2.5 or lower: Osteoporosis.
Other Diagnostic Tools and Medical Checks
In addition to the DEXA scan, a doctor can do additional examinations. Blood tests may be used to monitor levels of calcium, phosphorus, and vitamin D and to rule out other medical conditions that may cause bone loss. In some cases, a FRAX® score can be calculated. This is a computer model that estimates your absolute risk of a fracture over the next ten years based on your DEXA score and other clinical risk factors.
Prevention is Strength: Build and Maintain Strong Bones During and After Menopause
The best treatment for osteoporosis is prevention. While you have no control over genetics or age, you do have a significant impact on your diet, exercise habits, and lifestyle. It's never too late to start protecting your bones.
Nutrition as a Foundation: More than just Calcium and Vitamin D
A bone-healthy diet is the cornerstone of prevention. Two nutrients are central to this:
- Calcium: This mineral is the primary building block of bone tissue. Adult women need approximately 1000-1200 mg of calcium per day. Excellent sources include dairy products such as milk, yogurt, and cheese. Other good sources include green leafy vegetables (kale, broccoli), fortified plant-based milk, tofu, almonds and sardines (with bones).
- Vitamin D: This vitamin is essential for the absorption of calcium from the intestines. Without sufficient vitamin D, the body cannot use the calcium from food effectively. The main source is sunlight on the skin. In autumn and winter, and for people who spend little time outside, a supplement is often necessary. The Health Council recommends a daily supplement of 10-20 micrograms for women over 50.
In addition to calcium and vitamin D, other nutrients are also important, such as magnesium (in nuts, seeds, whole grain products), vitamin K (in green leafy vegetables) and proteins, which contribute to bone structure and muscle strength.
Movement: The Stimulus for Bone Growth
Exercise is a powerful stimulant for maintaining and even building bone mass. Bones respond to stress by becoming stronger. The most effective forms of exercise for bone health include:
- Weight-bearing exercises: Activities where your body works against gravity, such as brisk walking, jogging, climbing stairs, dancing, and tennis.
- Strength training: Exercises with weights, resistance bands or your own body weight (such as squats and push-ups) not only strengthen the muscles, but also exert positive pressure on the bones, which stimulates bone building.
- Balance and coordination exercises: Activities such as tai chi and yoga improve balance and stability, which is key to reducing the risk of falls.
Aim for at least 30 minutes of moderate-intensity weight-bearing exercise most days of the week, supplemented with two to three sessions of strength training.
Lifestyle Modifications for Optimal Bone Health
In addition to diet and exercise, a few other lifestyle adjustments contribute to strong bones:
- Stop smoking: This is one of the best things you can do for your overall health, including your bones.
- Moderate alcohol consumption: Limit your alcohol intake to a maximum of one glass per day.
- Maintain a healthy weight: Both underweight and overweight can have risks. A healthy BMI helps support bones.
Osteoporosis Treatment: Your Options and Strategies
When prevention has not been sufficient and osteoporosis has been diagnosed, active treatment is necessary to limit further bone loss and lower the risk of fractures. The treatment is often a combination of medication and lifestyle interventions. Unfortunately, in the Netherlands, you get half of women aged 50 and over have no effective secondary fracture prevention after an initial break up, highlighting the need for a proactive treatment strategy.
Drug Treatment: Slowing Bone Breakdown and Stimulating Bone Building
Drugs are often at the heart of osteoporosis treatment. The choice of a specific medication depends on the severity of the osteoporosis, your fracture risk and your medical history. The main classes of drugs include:
- Bisphosphonates: This is the most commonly prescribed group of drugs. They work by slowing down the activity of osteoclasts (bone degrading cells). As a result, the balance in bone structure is restored and bone density can stabilize or even increase slightly. Examples include alendronic acid and risedronic acid.
- RANK ligand inhibitors (Denosumab): This medication is given by a biannual injection and also inhibits the formation and activity of osteoclasts, but via a different biological mechanism than bisphosphonates.
- Selective Estrogen Receptor Modulators (SERMs): These medications, such as raloxifene, mimic the positive effects of estrogen on bone tissue without the risks associated with traditional hormone therapy on the breasts and uterus.
- Bone-building (anabolic) medication: In severe cases of osteoporosis, medication such as teriparatide may be prescribed. This medication actively stimulates osteoblasts to make new bones.
Non-Drug Strategies: Lifestyle as Integral Therapy
Lifestyle interventions are not only crucial for prevention, but also an indispensable part of treatment. Even when taking medication, the following elements remain vital:
- Adequate calcium and vitamin D: Your doctor will check that you are getting enough and prescribe supplements if necessary. Medication cannot do its job properly without these essential building blocks.
- Custom movement: A physical therapist can help set up a safe and effective exercise program that focuses on muscle strengthening and balance training to minimize the risk of falling.
- Fall prevention: This is a critical component of the treatment, as most fractures result from a fall.
The Synergy of Medication and Lifestyle: Optimal Results
The best result was achieved through a combined approach. Drugs slow down bone breakdown, while a healthy lifestyle provides the necessary building blocks and incentives for maintaining and strengthening bone. This synergy not only improves bone density, but also improves overall health, muscle strength and coordination, further reducing the risk of fractures.
Living with Osteoporosis: Practical Tips and Support
A diagnosis of osteoporosis does not mean the end of an active life. It does require awareness and adjustments in daily life to minimize the risk of fractures.
Preventing Fractures in Daily Life
Most osteoporotic fractures, particularly hip fractures, are caused by a fall. Fall prevention is therefore a top priority. A few practical tips:
- Make your home safe: Remove loose rugs, ensure good lighting (even at night), install handles in the bathroom and stairs, and remove cords and cables.
- Wear sturdy footwear: Opt for low-heeled shoes with a non-slip sole, both indoors and outdoors.
- Check your eyes: Have your eyes checked regularly. Impaired vision increases the risk of falling.
- Be aware of medication: Some medications may cause dizziness or drowsiness. Discuss any side effects with your doctor or pharmacist.
- Keep moving: Regular balance exercises and muscle strengthening workouts are the most effective ways to improve your stability and prevent falls.
Conclusion
The drop in estrogen accelerates bone loss, significantly increasing the risk of osteoporosis and disabling fractures. This guide has shown that you are not powerless, though. By understanding the mechanisms of bone loss and recognizing risk factors, you can take proactive steps to protect your skeleton.
The key message is that prevention is your most powerful weapon. A diet rich in calcium and vitamin D, combined with regular weight-bearing exercise and strength training, lays a solid foundation for strong bones. Avoiding smoking and excessive alcohol consumption further contributes to this.
For those who have already been diagnosed with osteoporosis, there is hope and effective treatment available. Modern medications can significantly slow bone degradation, while a continued focus on a bone-healthy lifestyle and fall prevention remains essential for minimizing fracture risks. The synergy between medical treatment and personal commitment leads to the best results.
Your next step is to turn this knowledge into action. Assess your own lifestyle and risk profile. Don't hesitate to discuss your bone health with your doctor, especially if you are menopausal or have multiple risk factors. Ask about the possibility of a DEXA scan. By taking control of your bone health, you are investing in a future of mobility, independence and vitality.
Lees meer blogs over de Menopauze
Inzicht en inspiratie voor vrouwen
Menovia
Meld je vandaag nog aan



