Menopause and Depression: How Hormonal Fluctuations Affect Your Brain and Change Your Mood

- Remove the existing class from the content27_link item to allow Webflow's native current state to be applied automatically.
- To implement interactions that allow sections in the table of contents to expand and collapse, select the content27_h-trigger element, add a trigger, and choose Mouse click (tap).
- For the first click, select the custom animation Content 28 table of contents [Expand], and for the second click, choose the custom animation Content 28 table of contents [Collapse].
- In the Trigger Settings, ensure that all checkboxes are deselected except for Desktop and above to prevent interaction issues on tablet and smaller devices.
The transition is often associated with physical symptoms such as hot flashes and night sweats. While these symptoms can be profound, there is a deeper, often invisible battle that takes place in a woman's brain. This is not a period of more physical discomfort; it is a fundamental neurological transition. The hormonal shifts that mark the end of childbearing years cause a cascade of changes in the brain that directly affect mood, cognition, and emotional resilience. For many women, this leads to an unwelcome introduction to mood swings, anxiety and, in severe cases, clinical depression. It is crucial to recognize this mental impact, not as a personal weakness, but as a direct result of a profound biological process that deserves proper attention and care.
Introduction: More than just hot flashes — The invisible impact on your brain
The menopause, or menopause, is much more than stopping menstruation. It is a period of intense change that affects every fiber of the body and mind. While hot flashes and sleep problems often predominate in conversations, the mental and emotional ones are psychological complaints often the hardest to understand and accept, both for the woman herself and her environment. Sudden irritability, persistent depression, or an overwhelming sense of anxiety are not a bad thing, but immediate symptoms of a brain adapting to a new biochemical reality.
The transition as a brain transformation: Hormonal shifts and their effects
During the transition, the brain undergoes significant adaptation. The hormones estrogen and progesterone, which played a crucial role in brain chemistry for decades, are declining dramatically. This forces the brain to find a new balance, a process that is sometimes described as a “recalibration.” This transition can temporarily lead to a disruption in communication between brain cells, which is reflected in a wide range of neurological and psychological symptoms. It is not an imagination; it is a measurable neurobiological process in which the brain learns to function with a different “operating system”.
The complex relationship between hormonal changes and mental health problems
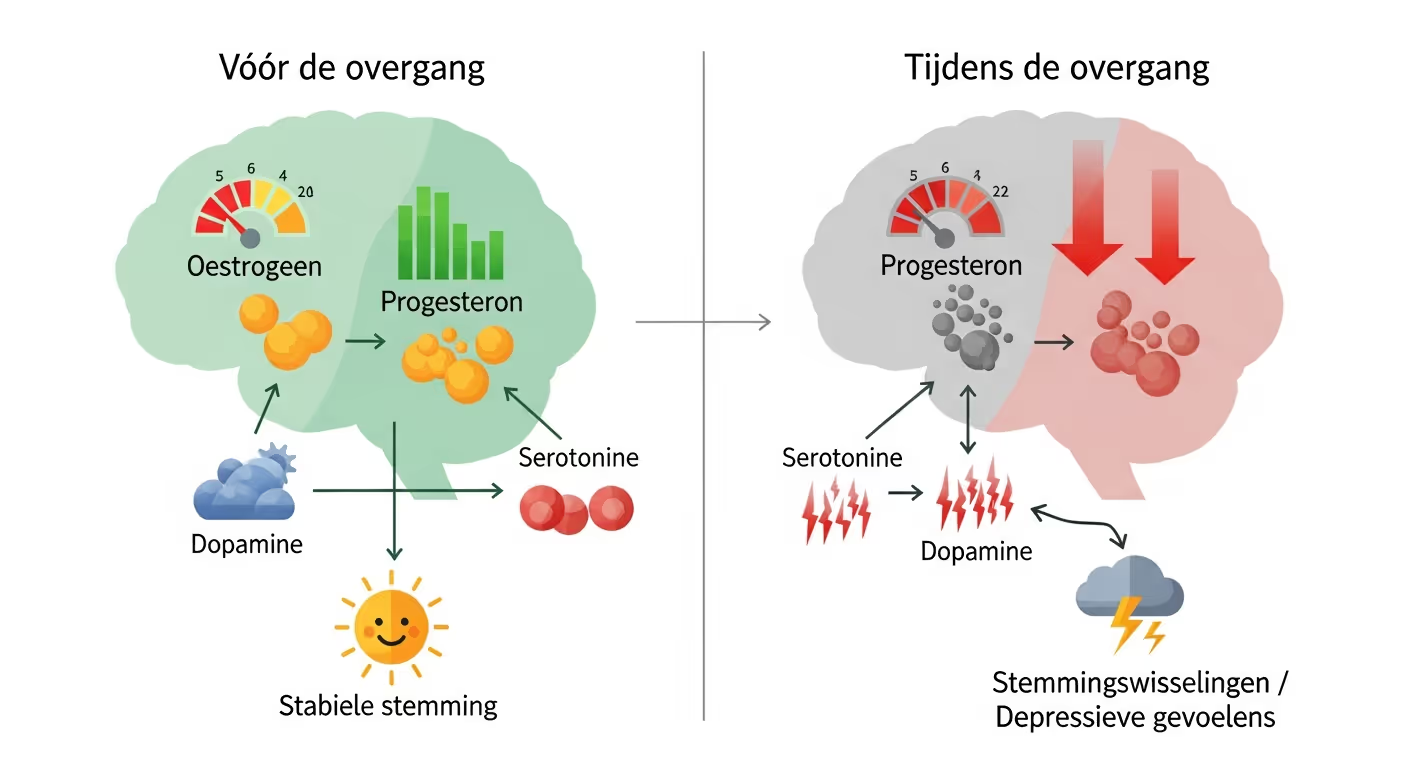
The decline in estrogen and progesterone during menopause disrupts the production of mood-regulating neurotransmitters, which increases the risk of depression and anxiety.
The link between declining hormone levels and psychological complaints is direct and complex. At home hormonal changes are not simple reproductive controls; they act as master controls in the brain, influencing everything from energy production to the production of mood-defining neurotransmitters such as serotonin and dopamine. When their influence wears off, the emotional stability that was previously taken for granted can falter. This explains why many women face intense ones for the first time in this phase. depressive feelings or anxiety, even if they've never experienced it before.
Why mental health in the menopause deserves special attention
The psychological impact of the transition has been systematically underestimated. Women are often told that it is “part of it” or that they should “get over it”. This trivialization is harmful and ignores biological reality. According to research, experiences up to 80% of women have menopausal symptoms, including depressive symptoms. It is a vulnerable period in which the risk of developing depression increases significantly. Timely recognition and serious attention to mental health, regardless of physical symptoms, are essential to the well-being of millions of women.
The Hormonal Earthquake: How Estrogen and Progesterone Affect Your Brain
To understand the mental symptoms during the transition, we need to look at the key players: the hormones that have shaped and supported the brain for decades. Their withdrawal causes a veritable earthquake in brain chemistry, shifting the fundamentals of your mood and cognition.
Estrogen: The driving force behind your neurotransmitters and brain functions
Estrogen is a powerful player in the brain. It has a protective and stimulating effect. This hormone promotes the production of serotonin, the neurotransmitter responsible for a stable mood and feelings of well-being. In addition, it stimulates the production of dopamine (motivation and pleasure) and acetylcholine (memory and learning). Estrogen also helps with the brain's energy supply by optimizing glucose uptake and even influences the biological clock, which regulates sleep-wake rhythms. When estrogen levels fall, these support weakens. Serotonin production may decrease, opening the door for depression and depression. The reduced energy supply can lead to the infamous “brain fog” and cognitive complaints.
Progesterone: The calming factor that disappears
Progesterone acts as the body's natural calming agent. In the brain, it is converted into a substance called allopregnanolone, which enhances the action of the neurotransmitter GABA (gamma-aminobutyric acid). GABA has an inhibitory, calming effect on the nervous system, helping to relax and promote sleep. The decline in progesterone during menopause leads to decreased GABA activity. This can result in increased irritability, anxiety, inner turmoil and serious sleep problems. The loss of this calming hormone makes the brain more susceptible to stress and panic.
Cortisol and the stress response: A double whammy for the brain
The decline in estrogen and progesterone has another adverse effect: it disrupts the regulation of the stress hormone cortisol. Estrogen normally helps control cortisol levels. When estrogen decreases, the body's stress response can become faster and more intense. This leads to chronically elevated cortisol levels, which further depletes the brain. High cortisol levels are associated with anxiety, depression, sleep disorders, and impaired memory. It creates a vicious cycle where hormonal fluctuations worsens the stress response, and the stress in turn intensifies menopausal symptoms.
The symptoms in your head: Recognizing depression and other mental symptoms
The biochemical changes in the brain manifest themselves as concrete, often confusing symptoms. It is important to recognize these as signals from an underlying hormonal imbalance, not as a personal failure. These complaints are just as real as the more visible ones. physical complaints.
Depressive feelings and depression: When is it more than a 'dip'?
Having a gloomy day is normal, but during the transition, these feelings can turn into persistent depression. Clinical depression is characterised by the duration and intensity of the symptoms. Symptoms include a persistently low mood, loss of interest or pleasure in (almost) all activities, feelings of worthlessness, and difficulty concentrating. For women with an existing condition such as a bipolar disorder, these hormonal shifts can further complicate mood swings and extra vigilance is needed. Like this depressive feelings Persisting for more than two weeks and interfering with your daily functioning, it is essential to seek help.
Anxiety, Panic, and Irritation: The Overactive Amygdala
The loss of the calming effects of estrogen and progesterone can make the amygdala, the brain's fear center, overactive. This can lead to a sudden increase in anxiety, panic attacks that seem to come out of nowhere, and a shorter fuse. For example, a hot flash can feel like a panic attack, complete with heart palpitations and a sense of loss of control, further fueling anxiety. This increased excitability is a direct neurological result of the hormonal changes.
The brain fog: Cognitive changes and memory loss
Many women experience “brain fog”: problems with concentration, word finding and short-term memory. This is not a sign of early dementia, but a direct result of reduced estrogen levels. Because estrogen supports communication between brain cells and the brain's energy supply, a deficiency can lead to slower information processing. While scary, these cognitive symptoms are usually temporary and often improve after menopause, when the brain has found a new hormonal balance.
Sleep problems and tiredness: A vicious cycle for your brain
Sleep is fundamental to mental health. During menopause, sleep is often disturbed by night sweats, a decrease in calming progesterone and an increased stress response. Chronic sleep deprivation has a disastrous effect on mood, cognitive function and emotional regulation. It makes the brain more vulnerable to negative thoughts and emotions, which significantly increases the risk of depression and anxiety. This tiredness creates a vicious cycle: poor sleep worsens mood symptoms, and the stress about it makes falling asleep even more difficult.
Why are you more vulnerable? Risk factors for depression during menopause
Not every woman develops depression during menopause. However, certain factors can increase vulnerability. Recognizing these risks is a first step towards prevention and timely intervention.
Previous episodes of depression or anxiety: An increased risk
One of the biggest predictors of depression during menopause is a history of mental health problems. Women who have previously experienced depression, post-natal depression or severe premenstrual mood symptoms (PMS/PMDD), especially during the luteal phase (the week before menstruation), are at increased risk. This suggests an underlying brain sensitivity to hormonal fluctuations. The use of hormonal contraception in the past and the response to it may also be an indication of this sensitivity.
Psychosocial factors and the phase of life: Transitional stressors
The transition often coincides with a phase of life full of stressors. Examples include caring for aging parents (informal care), children leaving home (empty nest syndrome), career changes or relational problems. These external stressors place an extra burden on a brain that is already working hard to adapt to a new hormonal reality. The combination of biological vulnerability and psychosocial pressure can overflow the bucket and the hormonal complaints aggravate.
Lifestyle factors: A strengthening or soothing effect
Lifestyle plays a crucial role in how the body and brain deal with the transition. Factors such as an unhealthy diet rich in sugar and processed foods, lack of exercise, excessive alcohol consumption and smoking can make the symptoms worse. Conversely, a healthy lifestyle can actually have a protective and soothing effect. A resilient body and brain are better able to cope with hormonal shifts.
Concrete steps for brain wellbeing: What can you do yourself?
While you can't stop hormonal changes, you do have an influence on how your body and mind respond to them. A proactive approach focused on lifestyle, nutrition and mental care can make a world of difference.
Lifestyle as a foundation for a resilient brain
- Power supply: Eat whole, unprocessed food. Focus on nutrients that support the brain, such as omega-3 fatty acids (fatty fish, flaxseed, walnuts), B vitamins (green leafy vegetables) and magnesium (nuts, seeds). Tryptophan, a precursor to serotonin, is found in bananas, turkey, and oatmeal.
- Movement: Regular exercise is a powerful antidepressant. It increases endorphins, improves sleep, and helps regulate stress response. A combination of cardio and strength training is ideal, with strength training also helping maintain bone density.
- Stress management: Techniques such as mindfulness, yoga, meditation, or deep breathing exercises can help calm the overactive nervous system and lower cortisol levels.
- Sleep hygiene: Create a calming bedtime routine. Avoid screens, caffeine, and alcohol in the evening and make sure your bedroom is cool and dark.
Supplements: Targeted support for your brain and mood
Some supplements can provide support, but always consult your doctor or an expert first.
- Omega-3 supplements: These can help reduce inflammation in the brain and support mood.
- Vitamin D: Essential for the mood, especially in the dark months. Deficiency is associated with an increased risk of depression.
- Magnesium: Can help with relaxation, reducing anxiety and improving sleep quality.
- Phytoestrogens: Substances from plants (such as soy or red clover) that have a mild estrogen-like effect and can alleviate symptoms for some women.
Professional help: When and where can you find it?
Self-care is important, but sometimes it's not enough. Don't hesitate to seek professional help. Your complaints are real, biological and treatable.
The doctor as the first point of contact: Recognize signals and make them negotiable
Your doctor is the first and most important point of contact. Prepare for your conversation: keep a journal of your symptoms (both physical and mental), note how they affect your daily life, and be clear about your request for help. Specifically ask if you hormonal complaints may be related to the transition, so that this is included as a possible cause.
Medical treatments and support
Depending on your symptoms and medical history, the doctor can suggest various options.
- Hormone replacement medication (HRT): Also known as hormone replacement therapy. Supplementing estrogen (and often progesterone) is the most effective treatment for both physical and mental complaints for many women. It can stabilize brain chemistry and significantly improve mood.
- Bioidentical hormones: These are hormones that are chemically identical to those of your own body. They are often customized and can be an alternative within HRT.
- Antidepressants: If depression is at the forefront of HRT is not an option, antidepressants (such as SSRIs) can help restore serotonin balance in the brain.
- GnRH injection: In very serious, specific cases (such as extreme PMDD that continues into perimenopause), a GnRH injection are being considered to temporarily shut down hormone production, which brings peace to the system.
It's also important to know that estrogen plays a protective role for the heart. Its decrease increases the risk of cardiovascular diseases, which may be an additional reason to consider treatment.
Psychological Support: Cognitive Behavioral Therapy and More
Therapy can be highly effective. Cognitive Behavioral Therapy (CBT) helps you recognize and break negative thought patterns that fuel depression. It can also provide practical tools for dealing with symptoms such as sleeping problems and hot flushes. More general mental support in the form of talk therapy or coaching can help to deal with the changes in this phase of life.
Specialized menopause clinics and centers of expertise
If your symptoms are complex or if you don't find the right help from your doctor, consider referring to a specialist menopause counselor, gynecologist, or a menopause clinic. Here you will find experts who have in-depth knowledge of the interaction between hormones, body and mind and can draw up a customized treatment plan.
Help with acute crisis
If you are dealing with an acute mental crisis or suicidal thoughts, seek help immediately. You are not alone. Contact your doctor, the GP office, or call the helpline anonymously and toll-free of charge at 113 Suicide Prevention via 0800-0113 or chat via 113.nl.
Conclusion: An informed path to mental wellbeing in transition
The transition is a period of profound change that can seriously test a woman's mental health. The link between declining hormones and depression is not a myth, but a neurobiological reality that requires serious attention.
Understanding the transition is the first step to recovery
Knowledge is power. By understanding that mood swings, anxiety, and feelings of depression are a direct result of changes in your brain, you can let go of guilt and shame. It is not a personal failure, but a biological process. This also applies to physical complaints axle sore breasts, stiff joints or changing sexual feelings; they are all part of the same hormonal imbalance. This knowledge enables you to take control of your health and well-being.
The importance of a proactive approach and multidisciplinary support
Waiting until the symptoms become unbearable is not necessary. A proactive approach, where you adapt your lifestyle, communicate openly with your environment and seek timely professional help, is the key to a better transition. The most effective approach is often multidisciplinary: a combination of medical support (such as hormone replacement medication), psychological guidance and targeted adjustments to your daily life. By taking these steps, you can not only meet the challenges of the transition, but also find a new, resilient balance for the phase of life that follows.
Lees meer blogs over de Menopauze
Inzicht en inspiratie voor vrouwen
Menovia
Meld je vandaag nog aan



