Menopause and Migraine: How Hormone Fluctuations Affect Your Headaches

- Remove the existing class from the content27_link item to allow Webflow's native current state to be applied automatically.
- To implement interactions that allow sections in the table of contents to expand and collapse, select the content27_h-trigger element, add a trigger, and choose Mouse click (tap).
- For the first click, select the custom animation Content 28 table of contents [Expand], and for the second click, choose the custom animation Content 28 table of contents [Collapse].
- In the Trigger Settings, ensure that all checkboxes are deselected except for Desktop and above to prevent interaction issues on tablet and smaller devices.
Introduction: Hormonal Turmoil and Your Headaches
The menopause is a phase of life that for many women involves a series of familiar symptoms, such as hot flashes and mood swings. A less discussed but significant issue is the change in headache patterns. Existing migraines can suddenly worsen, or headaches can become a serious complaint for the first time. This change is no accident; it is a direct result of the hormonal turmoil that the body is going through. Because migraines are one of the leading causes of disability among women worldwide, it's essential to understand this connection and what steps you can take.
The Transition: A New Phase of Life with Unexpected Complaints
The transition, or menopause, marks the end of the fertile period. It is a natural biological process, but the radical hormonal changes can significantly unbalance the body and mind. In addition to the known symptoms, the impact on neurological disorders such as migraines can be significant. The headache that occurs or worsens during this period is often described as hormonal headache, a specific type of headache that is directly linked to fluctuations in female hormones and requires a different approach than headaches caused by other causes.
Menopause and Migraine: A Common But Often Misunderstood Combination
The relationship between menopause and migraines is complex and frustrating for many women. While some women are experiencing a decrease in their symptoms, a significant group is actually noticing an increase in frequency and intensity. This paradox causes confusion and a sense of misunderstanding. It is crucial to realize that this is a familiar pattern. The unpredictability of hormone levels in the run-up to menopause (perimenopause) is often the biggest trigger for the worsening of these hormonal migraines.
What You'll Learn in This Article: Understanding, Recognition, and Practical Solutions
This article offers an in-depth insight into the relationship between menopause and migraines. We'll dive into the science behind hormonal headaches, explain how the different phases of the transition affect your migraine pattern, and help you recognize the specific symptoms. Finally, we discuss concrete treatment options and management strategies, from lifestyle changes to medical interventions, so that you can regain control and minimize the impact of these symptoms on your life.
The Hormonal Playing Field: The Influence of Estrogen and Progesterone
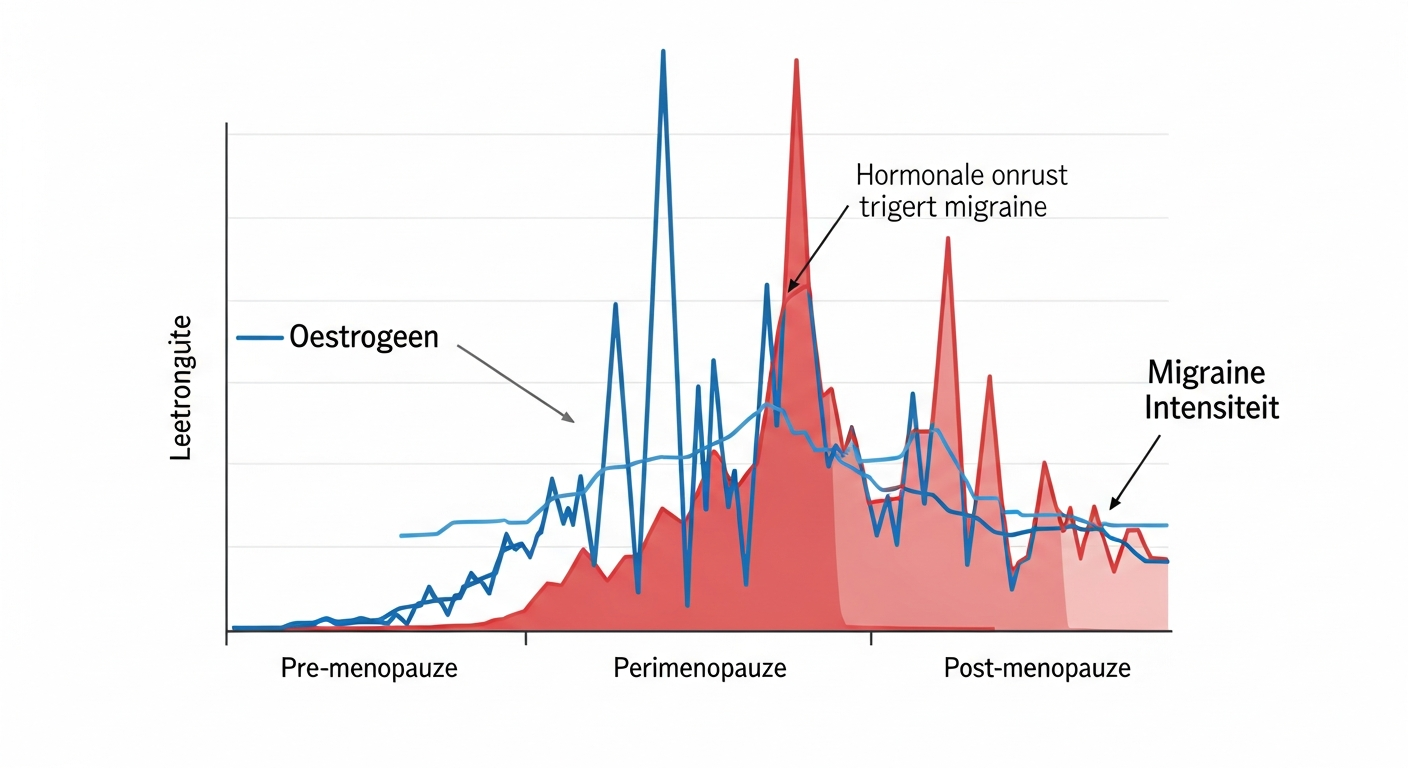
Perimenopause is characterized by unpredictable estrogen fluctuations. This “hormonal turmoil” is an important trigger for the increase in migraine symptoms. After menopause, when hormones stabilize at low levels, many women actually experience a decrease in their migraines.
To understand why menopause can affect headaches, we first need to look at the hormones that play a key role in the female cycle and health. This chemical compounds act as messengers that regulate countless processes in the body, including complex mechanisms in the brain that are involved in pain and migraines.
The Protagonists: Estrogen and Progesterone
Estrogen and progesterone are the two most important female sex hormones.
- Estrogen has a broad impact on the brain; it affects neurotransmitters such as serotonin, which play a role in mood and pain perception. It also helps keep blood vessels smooth and healthy.
- Progesterone generally has a more calming or stabilizing effect.
During childbearing years, levels of these hormones rise and fall in a predictable pattern. During the transition, this pattern becomes irregular and levels eventually fall permanently, disrupting brain balance.
Hormonal Headaches: A Definition
Hormonal headache is an umbrella term for headaches or migraines that are directly triggered by fluctuations in hormone levels. The most familiar form is menstrual migraine, which occurs during the sharp drop in estrogen just before or during menstruation. During the menopause, it is not the low estrogen level itself that causes the problem, but rather the erratic, unpredictable peaks and lows that overstimulate the brain and are a powerful trigger for a migraine attack.
The Connection to the Menstrual Cycle: A History of Hormonal Sensitivity
Women who are sensitive to hormonal headaches often notice this years before the menopause. If you were bothered by default: menstruation-related migraines whether menstruation-related migraines, your symptoms are more likely to worsen during the perimenopause. In more than half of female migraine patients, menstruation is an important trigger. This innate sensitivity to hormonal declines does not disappear, but is actually enhanced by the chaotic fluctuations that characterize the transition.
Why Women Are More Sensitive: The Role of Sex Hormones
The statistics are clear: migraines are about three times more common in women than in men. This difference largely occurs after puberty, when the production of sex hormones starts and the cyclic hormonal changes begin. The monthly fluctuations in estrogen and progesterone create periodic vulnerability to migraine attacks. Men do not have these hormonal cycles, which explains the lower prevalence of migraines among them. The menopause is in fact the last, and often most intense, phase of this lifelong hormonal influence on headaches.
The Transitional Phases: A Changing Migraine Pattern
The transition is not a single moment, but a process that consists of several phases. Each phase has a unique hormonal profile and can therefore have a different impact on your migraine. Understanding these phases can help explain the changes in your headache pattern and better anticipate what's to come.
Perimenopause: Erratic Hormone Fluctuations and Intensification of Migraines
Perimenopause is the period preceding the last menstrual period and can last four to ten years. This phase is characterized by extremely unpredictable hormone fluctuations. Estrogen levels can peak to higher than normal levels, only to fall sharply. It is precisely these abrupt declines that are a powerful trigger for hormonal migraines. Numerous clinical research confirms that women have a significantly increased risk of frequent headaches during perimenopause. For many women, this is the toughest period when it comes to migraine symptoms.
Menopause: Stabilization or Persistent Complaints?
Menopause itself is medically defined as the time when a woman has not had a period for twelve consecutive months. At this point, estrogen and progesterone levels have become consistently low. You would expect the headache to disappear then, because the trigger of the fluctuations will disappear. This is indeed the case for some women, but others continue to suffer from symptoms, possibly because their brain and blood vessels have yet to adapt to the new, permanently low hormone status.
Postmenopause: Often Improvement, But Not Always
After menopause, the postmenopausal phase begins. During this period, hormone levels are stably low. This is good news for the majority of migraine sufferers. Around two thirds of women with migraines without aura experience a significant improvement in their symptoms. The attacks become less frequent and less intense. For women with migraine with aura, the improvement is often less pronounced, and sometimes the symptoms remain unchanged.
How Hormone Levels Affect Headache Dynamics
In summary, the dynamics are as follows: high, stable estrogen levels (such as during pregnancy) often have a protective effect on the brain. Low, stable levels (such as in postmenopause) usually lead to improvement. It is the periods of instability and sharp declines (around menstruation and especially during perimenopause) that cause the biggest problems. The transition is therefore a temporary but potentially severe hormonal storm before calm returns.
Symptoms and Recognition: Distinguishing Menopausal Migraine
Recognizing migraines during menopause can be difficult, as symptoms can overlap with others physical complaints and psychological complaints. However, there are specific characteristics that can help make the correct diagnosis and link it to hormones.
Typical Migraine Symptoms: Headache, Nausea, and Hypersensitivity
The core symptoms of migraine remain the same regardless of the trigger. This includes unilateral, throbbing, or throbbing headache of moderate to severe intensity. The pain worsens with physical exertion. Common additional symptoms include nausea, sometimes with vomiting, and extreme sensitivity to light and sound (photophobia and phonophobia). An attack can last from hours to several days and is often disabling.
Specific Characteristics of Transitional Migraine Attacks
During the menopause, the pattern of migraine may change. Seizures may last longer, be more resistant to conventional medications, and more often start without a clear warning. They can also coincide with other menopausal symptoms, such as a hot flash or a period of intense tiredness. This interplay of symptoms sometimes makes it difficult to correctly identify the headache as a migraine.
Aura and Sensory Symptoms: A Warning Sign
Around a third of migraine sufferers experience an “aura” prior to the headache. An aura consists of fully reversible neurological and sensory symptoms that usually develop within an hour. The most common are visual disturbances, such as seeing bright lights, flickers, zigzags, or blind spots. Sometimes there are also sensory disorders (tingling in the arm or face) or speech problems. It is very important to distinguish migraine with aura, as this can influence the choice of certain treatments and the risk assessment.
Difference with Tension Headaches: Why the Right Diagnosis Is Crucial
Tension headaches are often confused with migraines. The main difference is the intensity and nature of the pain. Tension headaches feel like a tight, tight band around the head, are usually present on both sides and don't get worse with exercise. Nausea and hypersensitivity are generally absent. A correct diagnosis by a general practitioner or neurologist is crucial. Organizations like the Dutch Society for Neurology set guidelines to help doctors do this. Also, the expertise of the Dutch Association for Pediatric Neurology and the Dutch Association for Paediatrics in the field of headache diagnosis, underlines the importance of careful medical evaluation.
Other Menopausal Symptoms That Affect Headaches: Sleep Problems and Night Sweats
The transition involves a cascade of complaints that can indirectly trigger migraines. Bad sleep due to night sweats, hot flashes, or anxiety leads to fatigue, and sleep deprivation is a well-known, powerful trigger for migraines. The increased stress and mood swings that many women experience can further lower the threshold for a seizure. This creates a vicious cycle where menopausal symptoms and migraines reinforce each other.
The Biology Behind Pain: How Hormones and Brains Work Together
The pain of migraine isn't imaginary; it's a complex neurological disorder. Hormone fluctuations act as one of the most important modulators of this process. They influence the delicate balance of chemical compounds and structures in the brain that are involved in processing pain signals.
The Role of Neurotransmitters: Serotonin and Its Link to Migraine
Serotonin is a crucial neurotransmitter for mood, sleep, and pain regulation. Estrogen helps regulate serotonin levels in the brain. When estrogen levels fall, such as just before menstruation or during perimenopause, serotonin levels also fall. This decline can trigger a chain reaction within the trigeminal nervous system, leading to the widening of blood vessels in the meninges and the release of inflammatory substances. This results in the painful pulsation of a migraine attack.
Estrogen and Blood Vessels: The Vascular Influence on the Brain
Estrogen has a direct effect on the health and flexibility of blood vessels. It helps to keep the vascular walls relaxed and supple. A sudden drop in estrogen can lead to rapid contraction and subsequent dilation of blood vessels in and around the brain. This vascular instability is considered to be a key component in the development of migraine pain and may cardiovascular risk influence.
Triggers Beyond Hormones: Stress, Sleep Deprivation and Lifestyle
While hormones are a primary factor, migraines are rarely the result of a single trigger. Rather, it is a “threshold disease”. Hormonal fluctuations lower the migraine threshold, making you more sensitive to other non-hormonal triggers. Think of stress, irregular sleep patterns, skipping meals, certain foods (such as caffeine or alcohol), or even weather changes. Managing these lifestyle factors therefore becomes extra important during the transition.
The Complex Interaction between Hormone Balance and Headache Mechanisms
The relationship between hormones and migraines is not a simple cause-and-effect relationship. It is a complex interaction. Hormonal changes affect brain excitability, the sensitivity of pain receptors, the function of blood vessels, and the levels of important neurotransmitters. These combined effects create a perfect storm for migraine attacks to occur or worsen during menopause.
Treatment Options and Management: Getting Control of Menopausal Migraine
While menopausal migraines can be challenging, you're not powerless. A combination of lifestyle changes, the right medication and possibly hormonal therapy can significantly reduce the frequency and severity of the attacks. An open conversation with your doctor is always the crucial first step towards an effective treatment plan.
Lifestyle Modifications and Self-Care: The Basis for Prevention and Enlightenment
The most effective approach starts with you. A holistic approach, such as a fit & fabulous trajectory focused on wellbeing, can make a huge difference. Regularity is the key word here.
- Sleep & Stress: Aim for a consistent sleep schedule. Techniques such as cognitive behavioral therapy, mindfulness or yoga can help reduce the impact of stress.
- Food & Supplements: Eat regularly to keep your blood sugar levels stable. Some studies suggest that supplements such as coenzyme Q10 and vitamin D can play a preventive role in migraine. Talk to your doctor before taking supplements.
- Movement: Regular, moderate exercise (such as walking or swimming) can reduce the frequency of seizures.
- Expertise: A holistic approach can be further supported by institutions that specialize in lifestyle and well-being, such as the MOOI Institute, where one looks at the overall balance of the body.
Drug Treatment: Attack and Preventive Therapy
The drug treatment for migraine consists of two pillars, which you always decide in consultation with your doctor.
- Seizure treatment: You take this medication as soon as you feel an attack coming on. This starts with simple pain relievers, but often specific migraine medications such as triptans are more effective.
- Preventive treatment: If you have frequent seizures, preventative medication may be considered. These are medicines that you take daily to reduce the risk of an attack. For chronic, difficult-to-treat migraines, treatment with botulinum toxin (botox) are an option.
It is very important to avoid overuse of pain relievers in order to medication overuse headache to prevent, a chronic headache caused precisely by the medication.
Hormonal Therapies: A Targeted Approach to Hormonal Headaches
For headaches that are clearly hormonally triggered, hormone replacement therapy (HRT) may be an option. By stabilizing estrogen levels, HST can remove the trigger for the sharp declines. However, this does not work for everyone and can actually make migraines worse for some women. A crucial warning applies to women with migraines with aura. The use of oral contraception whether oral contraceptives that contain estrogens, as well as oral HRT, are often not recommended for them. Clinical research has shown that this is the risk of cardiovascular diseases, and in particular on cerebral bleeding (stroke), light may increase. Transdermal administration (via a patch or gel) is often preferred because it cardiovascular risk seems to affect less. Always consult extensively with your doctor or gynecologist about the pros and cons of hormonal contraception and HST in your specific situation.
Conclusion
The link between menopause and migraine is unmistakable and rooted in the complex interaction between hormones and the brain. Perimenopause is often the most challenging period, in which erratic estrogen fluctuations can increase the frequency and intensity of headaches. While this can be a daunting experience, it's important to remember that this phase is temporary. For the majority of women, the stable hormonal rest of postmenopause offers significant relief.
The key to managing menopausal migraines lies in taking a proactive and informed approach. Recognizing the symptoms and understanding your triggers are the first step. Consult your doctor to make a correct diagnosis and create a personalized treatment plan. This plan can include lifestyle changes, the right medication and careful consideration of hormonal therapies. By taking control of your health, you can minimize the impact of migraines and maintain a high quality of life during the transition.
Medical disclaimer: The information in this article is for informational purposes only and does not replace professional medical advice. Always consult a qualified physician or healthcare provider for diagnosis and treatment of medical conditions. Never stop or change a treatment without talking to your doctor.
Lees meer blogs over de Menopauze
Inzicht en inspiratie voor vrouwen
Menovia
Meld je vandaag nog aan



