Menopausal symptoms by phase: Recognize symptoms from perimenopause to postmenopause
- Remove the existing class from the content27_link item to allow Webflow's native current state to be applied automatically.
- To implement interactions that allow sections in the table of contents to expand and collapse, select the content27_h-trigger element, add a trigger, and choose Mouse click (tap).
- For the first click, select the custom animation Content 28 table of contents [Expand], and for the second click, choose the custom animation Content 28 table of contents [Collapse].
- In the Trigger Settings, ensure that all checkboxes are deselected except for Desktop and above to prevent interaction issues on tablet and smaller devices.
The menopause, also known as a climacterium, is a natural phase of life that every woman goes through. It is a period of profound hormonal changes that can cause both physical and emotional complaints. While many women are familiar with terms such as menopause and hot flashes, the process of the transition is far more complex and involves different phases, each with their own specific symptoms. In the Netherlands, more than one million women aged 40 to 60 experience the transition every year, of which as many as 80% experience complaints [Guidelines Database, 2025]. Recognizing the symptoms per phase is essential to make this transition as smooth as possible and to make conscious choices for your well-being. This phase can last a total of 5 to 10 years, with an average duration of six to seven years [A.Vogel, 2026]. Understanding these changes prepares you for the challenges of this hormonal journey, from the silent start to life after the last period.
Understanding the Menopause: A Hormonal Journey
The transition is more than just the end of menstruation; it's a gradual process driven by declining hormonal activity. The ovaries, which estrogen and progesterone produce, fewer of these essential hormones begin to be produced. This one hormonal changes are the fundamental cause of the symptoms experienced by women. Understanding the precise role of these hormones and the changes in their production is crucial to understanding the complexity of the transition. A visual overview of this hormonal journey, from the first fluctuations in the perimenopause to the new hormonal balance in the postmenopause, is essential for self-knowledge.
What is the Transition (Climacterium)?
The term transition, or climacterium, encompasses the entire period of hormonal changes which leads to the permanent cessation of the menstrual cycle. It is a natural biological process, not a disease. During this phase, the ovaries gradually undergo a change in their function, resulting in a fluctuation and ultimately a decline in the production of estrogen and progesterone. This decrease affects various body functions and can cause various menopausal symptoms. This period can last a total of 5 to 10 years, with an average duration of six to seven years [A.Vogel, 2026].
The Crucial Role of Hormones: Estrogen and Progesterone
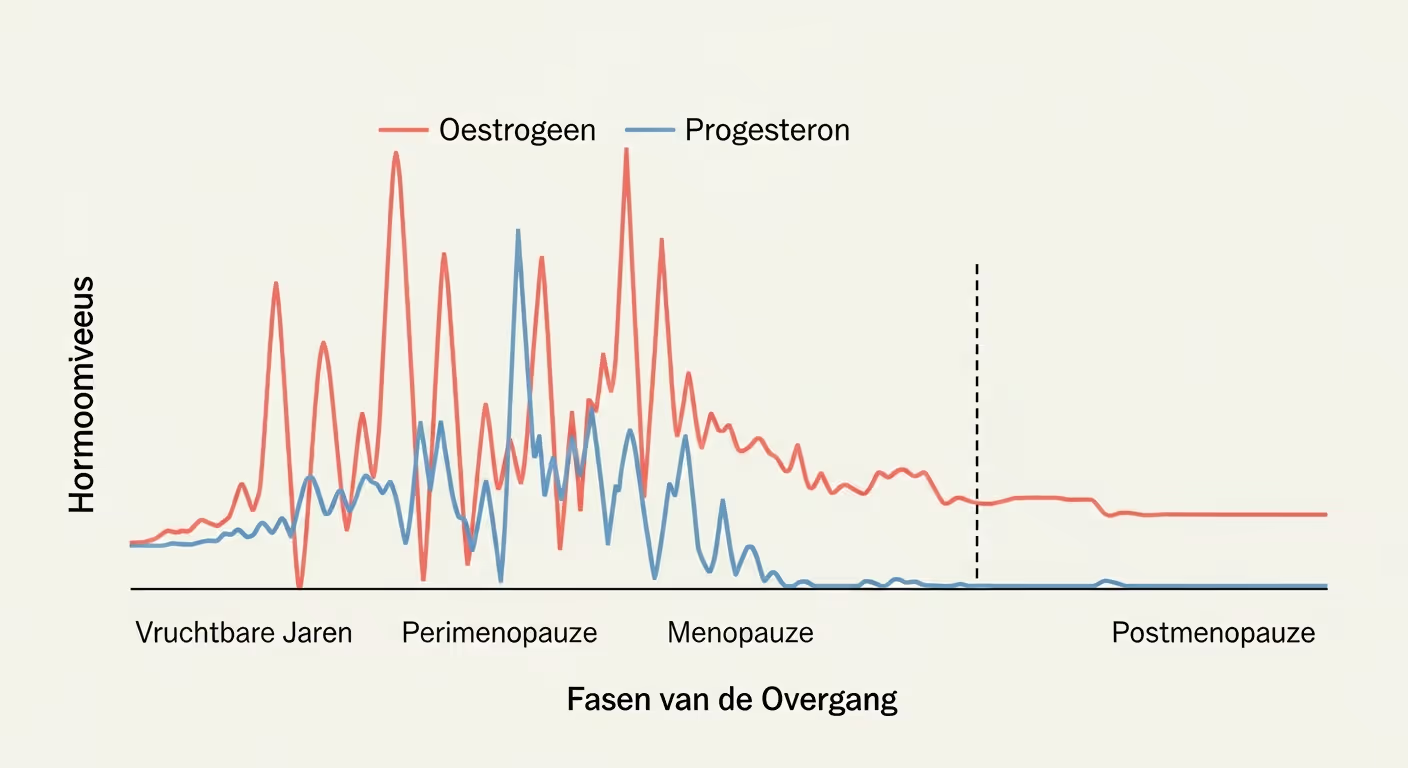
The hormonal journey: Estrogen and progesterone levels fluctuate sharply during perimenopause and stabilize at low levels after menopause.
Estrogen and progesterone are the two most important female hormones that play a central role during the reproductive years and beyond. Estrogen is responsible, among other things, for regulating the menstrual cycle, maintaining bone density, skin elasticity, and regulating body temperature. Progesterone prepares the body for a possible pregnancy and plays a role in sleep and mood. As women age, ovaries start less estrogen and progesterone to produce. These fluctuations and decreases in hormone levels are the immediate cause of many of the well-known menopausal symptoms, such as hot flashes and mood swings. The precise changes in the hormone balance partly determine the severity and nature of the symptoms, and the achievement of a new hormonal balance is a key to wellbeing.
Why Phase Layout Is Essential for Recognition
The transition is not a sudden event, but a gradual process that can extend over many years. Dividing this period into different phases — premenopause, perimenopause, menopause and postmenopause — makes it easier to recognize the specific changes and associated symptoms. Each phase has its own dynamics in hormone levels and associated symptoms. Without this phasing, it is difficult to understand why certain complaints suddenly appear to arise or change. The correct division into a phase provides a framework for self-insight and makes targeted approaches to menopausal symptoms possible.
Phase 1: Premenopause — The Silent Start
Premenopause is the period preceding the actual perimenopause. It is often the quietest phase, where the changes are subtle and people are usually not aware that the transition is approaching. This phase can begin as early as the 35th or 40th year of life, depending on genetic factors and lifestyle. It is the phase in which the body's own production of hormones is still relatively robust, but the first, barely noticeable, fluctuations can occur.
What happens in this phase?
In premenopause, the ovaries still function mostly normally, and the hormone levels — especially estrogen and progesterone — are relatively stable and cyclical. The menstrual cycle is still regular, although very mild irregularities can already occur in some cases. Fertility is slowly beginning to decline, but conception is still quite possible. The changes here are still minimal, so the transition from this phase to the next often goes unnoticed.
Recognizing Subtle Symptoms
Premenopausal symptoms are often so mild that they are easily attributed to stress, fatigue, or other factors. Some subtle signs may include a slight change in menstruation (e.g. slightly shorter or longer cycles), mild mood swings, or a slight decline in energy. Sometimes a beginning skin change can also occur, such as a little more dryness. Here are the first hints of hormonal changes, even before the more obvious symptoms of perimenopause occur.
Phase 2: Perimenopause — The Most Dynamic Period
Perimenopause is the longest lasting phase characterized by the most pronounced and dynamic hormonal changes. This period can last for many years, sometimes up to 10 years, and only ends with menopause. It is the phase where most women notice the first obvious menopausal symptoms. Women may wonder if their complaints in case of menstruation can point to more, and that is often a harbinger indeed.
Early Perimenopause: First Clear Signs
In early perimenopause, the ovaries start less consistently estrogen and progesterone to produce. This leads to noticeable fluctuations in hormone levels. The most obvious sign is often a changing period. The cycles may become shorter or longer, the bleeding may be heavier or lighter. In addition to menstrual changes, the first hot flashes and night sweats perform. Women may also experience more mood swings, irritability, sleep problems and declining skin elasticity, leading to increasing dryness. The number of women using hormone therapy increased by 76% in 2023 compared to 2018 [Stichting Pharmaceutical Key Numbers, 2024], underlining the increase in recognition and the search for solutions in this phase. The first ones can also psychological complaints manifest themselves.
Late Perimenopause: Intensification of Complaints
As perimenopause progresses, the hormonal changes even bigger. The fluctuations in estrogen and progesterone become more extreme, leading to an intensification of symptoms. Hot flushes can become more frequent and more severe, night sweats can significantly disrupt sleep, and mood swings can go deeper, sometimes bordering on feelings of depression. In addition to the well-known complaints such as fatigue and concentration problems, vaginal ones are also vagina moistdryness (or dryness) is a common complaint, partly due to declining estrogen production. The skin becomes thinner and drier, and libido may decline. This can lead to a awkward moment, for example when you're less comfortable in social situations or intimate moments. Many women find that they more often things need to adapt to their energy levels or physical discomfort. In this late perimenopause, many women experience significant menopausal symptoms that can affect their daily lives. It is important to realize that many of these complaints are not 'normal' with age, but are an expression of the changing hormonal balance.
Phase 3: Menopause — The Official Moment
Menopause marks a specific point in the transition period: the time when menstruation has finally stopped. It is not a gradual transition, but a clear milestone that will be determined afterwards. It is the point at which perimenopause transitions into postmenopause.
The Definition of Menopause
Menopause is officially diagnosed when a woman has not had a period for twelve consecutive months. The average age at which this occurs is around 51 to 52 years in the Netherlands. This moment is the result of the complete cessation of follicle maturation in the ovaries, causing the production of estrogen and progesterone almost comes to a standstill. It's important to remember that menopause is the highlight of the transition, not the end of it.
What does this mean for complaints?
When menopause is reached, it means that the most extreme hormonal fluctuations of perimenopause are over. Hormone levels stabilize at lower levels. This means that some symptoms, such as intense hot flashes and irregular periods, may decrease or even disappear. However, the lower estrogen levels cause other complaints, such as vaginal vagina moistDryness, decreased libido and skin changes may persist or even worsen. The body has now entered a new hormonal balance, which comes with its own challenges.
Phase 4: Postmenopause — Life After the Last Menstruation
Postmenopause begins after the definitive menopause and lasts for the rest of life. It is the phase in which the body adapts to a permanently low level of estrogen and progesterone. Although the dynamic hormonal changes are over, this phase presents specific challenges and changes, with an increased risk of certain health problems such as cardiovascular diseases.
Persistent and New Complaints
In the postmenopause, many symptoms that arose during the perimenopause, such as vaginal dryness, thin skin, and decreased libido, often persist. The absence of estrogen has long-term effects, including an increased risk of osteoporosis and an increased risk of cardiovascular diseases. Women may also continue to suffer from joint pain, trouble sleeping and dry eyes or mouth. The skin continues to thin and lose elasticity. It is a time when it is important to pay attention to long-term health and to optimize well-being so that women can continue their lives as vitally as possible. The skincare requires extra attention,. The need for a healthy lifestyle becomes even clearer here.
Recognize Your Phase: Tools and When to See a Doctor?
Recognizing the phase you are in is crucial for effectively addressing menopausal symptoms. Fortunately, there are various tools available to help you with this, and it's important to know when professional help is needed. Self-knowledge is the first step towards creating a new hormonal balance.
Self-Recognize: Symptom Tracking and Questionnaires
Keeping track of symptoms can be a valuable tool for recognizing patterns and gaining insight into your own transition process. Keeping a diary where you record your symptoms every day — such as hot flashes, periods, sleep patterns, mood and energy levels — can help identify the phase. By documenting these changes, you can better understand what's happening in your body. Women who are in the perimenopause can thus recognize the subtle signs that their complaints in case of menstruation can point to this phase.
When Do You Seek Professional Advice?
Although the transition is a natural process, the symptoms can sometimes be so severe that they affect your daily life. Don't hesitate to seek professional advice from your doctor, gynecologist or a specialist doctor at Menovia. This is particularly recommended when:
- Severe or frequent hot flushes that seriously interfere with sleep and function.
- Serious mood swings, depressive feelings or anxiety (psychological complaints).
- Persistent vaginal dryness that leads to pain when having sex.
- Unexpected blood loss, prolonged or very heavy periods, or blood loss outside the menstrual period.
- Concerns about your bone health or cardiovascular risks.
The importance of professional help is underlined by the increased use of hormone medications: around 130,000 women used hormone medication in 2024 [NPO Radio 1, 2025], which shows the growing recognition of the impact of the transition. Menovia can advise you on the right thing medical research and possible treatment options, including bioidentical hormones.
Diagnostics: Blood Tests and Hormone Levels
Diagnosis of menopause is often based on the symptoms and age of the woman. Blood tests may be useful, but results should be interpreted with caution. Hormone levels, such as FSH (follicle-stimulating hormone) and estrogen, can fluctuate significantly, especially in the perimenopause. A high FSH value may indicate decreased ovarian function, but this is not always unambiguous, especially in the early phases. A doctor will usually use a combination of complaint history, age and possibly blood tests to understand the phase you are in and determine the best treatment options.
Dealing with Complaints: Solutions and Lifestyle Advice per Phase
Dealing effectively with menopausal symptoms requires an integrated approach that is tailored to the specific phase you are in. Lifestyle plays a crucial role, supplemented with targeted medical treatments where necessary. One healthy lifestyle is the basis for well-being during the transition.
Lifestyle as a Basis: A Healthy Lifestyle for Every Phase
One healthy lifestyle forms the basis for well-being during the transition. This includes a balanced diet rich in vegetables, fruits and whole grain products, drinking enough water, regular exercise (both cardio and strength training to support bone and muscle health), and adequate sleep hygiene. Stress management techniques such as mindfulness, yoga, or meditation can help reduce hot flashes and mood swings. These basic principles apply to all phases, but the emphasis may shift. In the perimenopause, the focus can be on managing fluctuating energy levels, while in the postmenopause, attention can be more focused on maintaining bone density and cardiovascular health. Of the 80% female employees who sometimes or regularly experience hormone-related complaints, 35% hide them at work [TNO and CBS, 2025]; they may benefit from these lifestyle recommendations, which can reduce the impact on work.
Medical Treatments: Options and Trade-offs
In addition to lifestyle interventions, various medical treatments are available for women who suffer from severe menopausal symptoms. Hormonal therapy (HT) is a commonly used option to estrogen and sometimes to supplement progesterone. Around 130,000 women used hormone medications in 2024 [NPO Radio 1, 2025], demonstrating its popularity and effectiveness. HT can cause hot flashes and night sweats significantly reduce, and also help with vaginal dryness and osteoporosis. The choice for HT depends on individual medical history, symptoms and preferences and should always be made in consultation with a physician. Local treatments (e.g. with estrogen) are effective for vaginal dryness and urination problems. Some women choose bioidentical hormones, which are identical in molecular structure to the body's own hormones, for a personalized approach.
Specific Skin Care Tips
The skin undergoes significant changes during menopause, mainly due to the declining estrogen mirrors. The skin becomes thinner, drier, and loses elasticity, leading to more wrinkles and increased sensitivity. In perimenopause and postmenopause, targeted skin care is essential. Use gentle, hydrating cleansing products and rich moisturizers that contain ingredients such as hyaluronic acid, ceramides, and peptides. Protect skin from the sun daily with a high SPF to prevent premature aging. Consider anti-oxidant products to protect skin from damage. Women who suffer from vaginal dryness may benefit from specific lubricants or moisturizers.
Practical Support and Apps
In addition to medical and lifestyle interventions, practical support can make a big difference. There are tons of apps available that help track symptoms, provide relaxation and sleep exercises, or offering information about the transition. Online communities and peer groups can be a valuable source of support and recognition. Sharing experiences with other women who are going through the same phase can help you feel less alone and gain new insights. Education about the transition is the first step towards empowerment. Healthcare providers such as Care for Women provide specialized support. It is always advisable to discuss its use with your doctor or an expert, especially in combination with other medications or therapies.
The transition is a complex but natural phase of life that can have a significant impact on women's lives. By understanding the different phases — premenopause, perimenopause, menopause, and post-menopause — and recognizing the specific symptoms, women gain the key to self-knowledge and control. The hormonal changes, in particular the fluctuations and declines of estrogen and progesterone, are the cause of complaints such as hot flashes, mood swings, and changes in the skin and mucous membranes, including dryness.
Recognizing subtle signs in premenopause, the dynamic changes during perimenopause, the official time of menopause, and the ongoing impact in postmenopause enables women to act proactively. The 5 phases of the transition provide a clear structure for placing these changes.
The impact of the transition on daily life, including work, as figures show that 71% of women with menopausal symptoms find it difficult to combine work and 73% say they are less productive [NOS, 2024], requires more openness and understanding.
Lees meer blogs over de Menopauze
Inzicht en inspiratie voor vrouwen
Menovia
Meld je vandaag nog aan